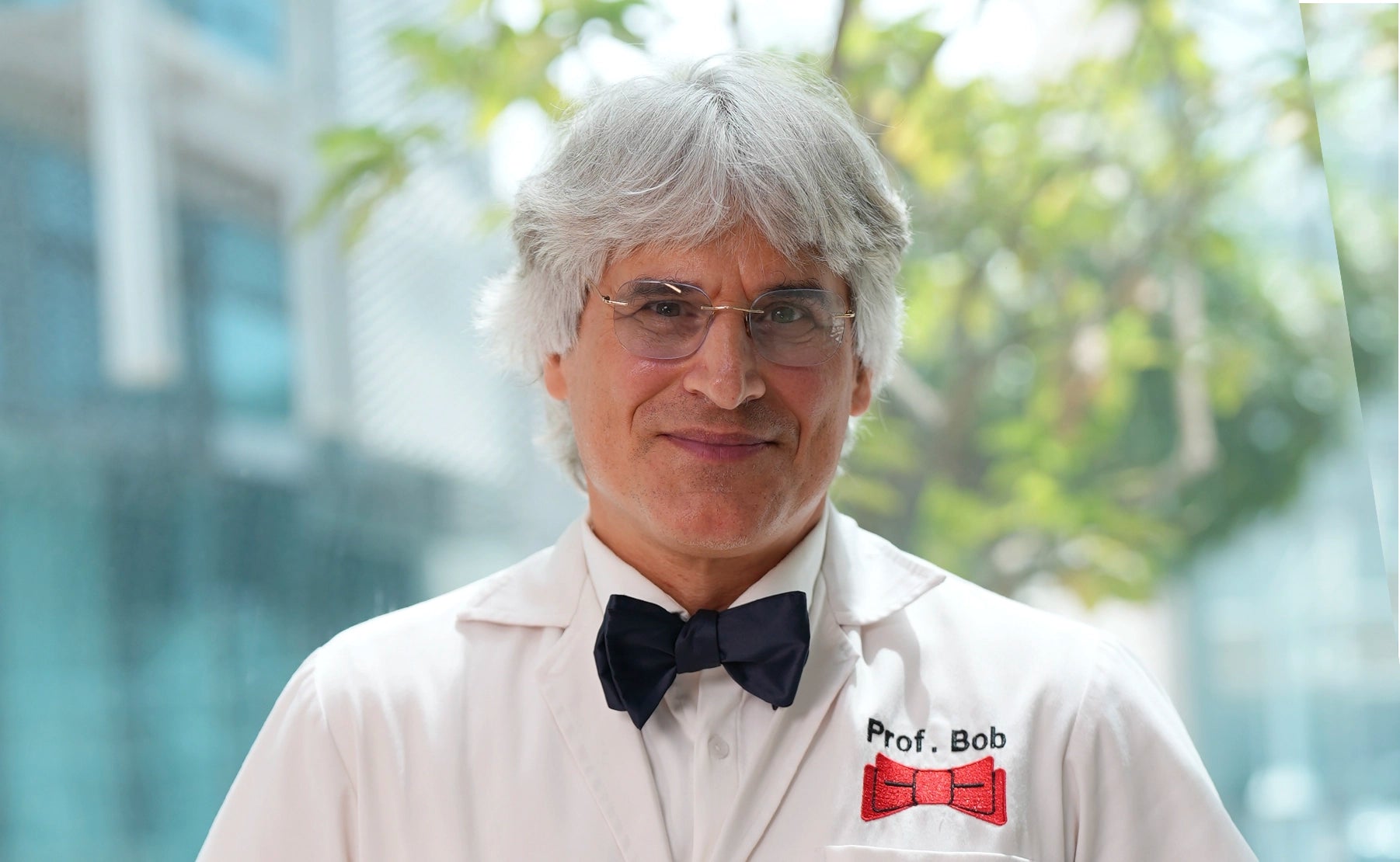
Prof. Dr. Robert Hierner at a glance.
FAQs for Peripheral nerves & Brachial Plexus
Peripheral nerves can be compared to highly sophisticated cables, that relay information between your brain and the rest of your body. Prof. Dr. Robert Hierner is a reference in the field of interdisciplinary and multi-professional treatment of peripheral nerve lesions.
What are the reasons for peripheral Nerve Injuries?
Peripheral nerves can be damaged in several ways:
- Injury by cut, crush or acute and chronic (Carpal Tunnel syndrome) compression
Infection (leprosity/Hanson`s disease, …) - Metabolic Disorders: Diabetes, mucopolysaccharoid, …)
- Medical conditions: Pregnancy, Renal failure (dialysis patients), …)
- autoimmune Diseases (Guillain-Barre syndrome, Lupus, Rheumatoid arthritis and Sjogren's syndrome, ….)
- Intoxications, ……
Symptomes of peripheral nerve lesions
Peripheral nerves may have motor, sensory and autonimic functions, which may be impaired to different degrees.
Motor function
Damage to these nerves is typically associated with
- muscle weaknes (palsy)
- muscle cramps
- uncontrollable muscle twitching
Sensory function
Damage to sensory nerves is typically associated with:
- altered touch
- alterted temperature
- pain
Autonomous function
Damage to autonomic nerves can be associated with activities that are not controlled consciously, such as
breathing, the heart, thyroid function, and digestion, which can result in secondary complications secondary to:
- excessive sweating
- changes in blood pressure
- inability to tolerate heat
- gastrointestinal symptoms
How can peripheral nerve lesions be managed ?
Multidisciplinary Patient Care: Only through an intensive interdisciplinary Cooperation can achieve an optimal therapy result be reached. Therapy team members are :
- Hand Surgery (often in conjunction with the neuropathologist)
- Physiotherapy
- Neurology
- Radiology
- Anesthesia & Pain Clinic (deafferentation pain, causalgia, …)
- Internal Medicine (Diabetes, Dialysis)
- Social services/employment office/professional association (professional rehabilitation or reintegration)
- orthopedic technician (sleeve and splint apparatus)
- Mental support
- Patient support groups
The constant exchange of information (Telephonec alls, doctor's letters) within the team is exceptional Importance. An optimal treatment result can only be achieved if all members of the therapy team work together seamlessly.
Ask the Expert: Peripheral Nerves
The right therapy at the right time, helping nature to correct during growth, and secure as many hand functions as possible.
Acute Nerve Injury
Acute nerve injuries can leed to 2 situations:
- Lesion with continuity loss
- Lesion-in-continuity
Peripheral nerve reconstruction with the aim of improving motor skills should be carried out no later than 12
(large distance, i.e. proximal lesion) or a maximum of 18 months (small distance, distal lesion), as the endorgan muscle will undergo irreversible degenerative changes with muscle denervation. If improvement in (protective) sensitivity is to be achieved, an nerval reconstruction can still be carried out after
24 – 36 months.- Lesion with continuity loss
– In cases with clear cut and no nerve tissue loss, microsurgical tension-free nerve suture (nerve
coaptation) is performed.
– In cases with loss of nerve tissue, reconstruction of the nerve gap can be performed using
several techniques, such as nerve tubes or nerve grafts taken from the patient (autologous) - Lesion-in-continuity. In cases of preserves continuity, standardized clinical and neurophysiological examinations are
mandatory, for at least 3 – 6 months. Depending on the quality of nerve regeneration, different forms of nerve reconstruction as necessary
Postoperatively the coaptation must be protected for 10- 14 days by immobilization. Heavy work and impact action can be resumed after 6 weeks. The higher the nerve lesion, the longer regeneration time (1mm a day). At the hand level, nerve regeneration needs 6 – 12 months
Chronic Nerve Compression (Carpal Tunnel Syndrome)
What causes carpal tunnel syndrome?
Nerve compression syndrome - also known as nerve entrapment syndrome - is a chronic nerve lesion. It occurs where peripheral nerves pass through anatomical narrows bounded by rigid structures. Factors such as metabolic disorders (diabetes, pregnancy, mucopolysacharoidosis, ...) or toxic factors (dialysis, ...) favor the occurrence of compression syndromes. In case of arthritic changes at the cervical spine with beginning nerve root compression (radicular compression) the peripheral compression syndrome can be inhanced (“double crush syndrome”).Carpal Tunnel Syndrome, which is the entrapment syndrome of the median nerve at the wrist level – is the most common chronic compression syndrome in humans. Nearly 50% of all humans will experience more or less carpal tunnel syndrome during aging.
Other frequent chronic nerve compression
syndromes in the arm are:- Posterior interosseous nerve syndrome
- Sulcus ulnar nerve syndrome
- Thoracic outlet syndrome (TOS)
What are the Symptoms of Carpal Tunnel Syndrome?
The resulting functional disorder depends on the extent and duration of the constriction. It can range from slight discomfort (“hands go to sleep”) to a minor motor weakness (increasing clumsiness) to complete (senso motor) paralysis. Nocturnal pain is also typical, waking the patient up and causing him to shake his/her hands or let him/her hang down from the bed.
How can you treat carpal tunnel syndrome?
Nerve lesions of any kind need a full neurological work-up. For the treatment of carpal tunnel syndrome we are using the "Integrative Therapy Concept according to BERGER”. The goal of treatment is to relieve the pain and restore normal sensibility and grip function, by:- Prevention and Awareness
- Conservative (non-operative) treatment
- Operative treatment
Old nerve lesion (longstanding nerve palsy)
Complete nerve lesions lead to irreversible changes at the muscles (motor function) after 12 to 18 months and nerve receptors (sensory function) after 24 – 36 months. Beyond this timeframe, there is no useful function results to be expected from nerve repair/reconstruction. For these cases secondary reconstructive methods are used.
- Secondary muscle function reconstruction
- Secondary sensory function reconstruction
Brachial Plexus Lesion
Acquired brachial plexus lesions may be caused by
- acute trauma
- post-traumatic lesions of adults
- birth trauma in babies (Obstetrical brachial Plexus Lesions/OPBL)
- chronic damage by compression (thoracic outlet syndrome/TOS)
- Radiation-induced brachial plexus neuropathy (RIBPN) (in breast cancer)
- Tumor-induced brachial plexus
neuropathy (TIBPN) (lung/Pancoast cancer, breast, ..) - others (inflammation, …….)







